

















In order to make the diagnosis of ARVC, a number of clinical tests are employed, including the electrocardiogram (EKG), echocardiography, right ventricular angiography, cardiac MRI, and genetic testing.
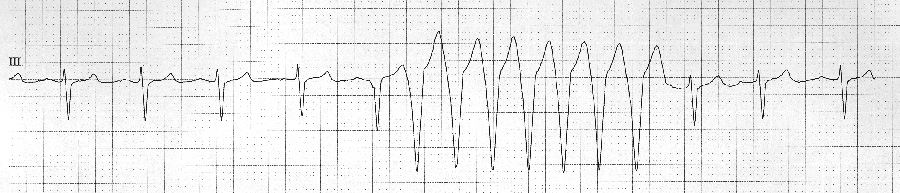
Most individuals with ARVC have some EKG abnormality. The most common EKG abnormality seen in ARVC is T wave inversion in leads V1 to V3. However, this is a non-specific finding, and may be considered a normal variant in right bundle branch block (RBBB), women, and children under 12 years old.
RBBB itself is seen frequently in individuals with ARVC. This may be due to delayed activation of the right ventricle, rather than any intrinsic abnormality in the right bundle branch.
The epsilon wave is found in a small proportion of patients with ARVC. This is described as a terminal notch in the QRS complex.
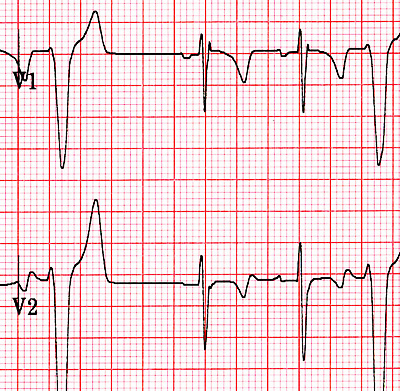
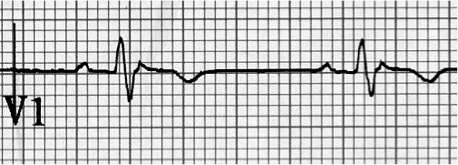
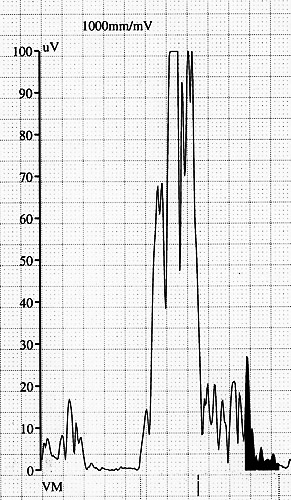
It is due to slowed intraventricular conduction. The epsilon wave may be seen on a surface EKG; however, it is more commonly seen on signal averaged EKGs.
Slurring of the upslope of the S wave, so called terminal activation delay (TAD, normal < 55 msec), is seen in the anterior precordial leads (V1-V3), which is a recently added criterion for ARVC in the new Task Force Criteria.
Ventricular ectopy seen on a surface EKG in the setting of ARVC is typically of left bundle branch block (LBBB) morphology, with a QRS axis of -90 to +110 degrees. The origin of the ectopic beats is usually from one of the three regions of fatty degeneration (the "triangle of dysplasia"): the RV outflow tract, the RV inflow tract, and the RV apex.
Signal averaged ECG (SAECG) is used to detect late potentials and epsilon waves in individuals with ARVC.
Echocardiography may reveal an enlarged, hypokinetic right ventricle with a paper-thin RV free wall. The dilatation of the RV will cause dilatation of the tricuspid valve annulus, with subsequent tricuspid regurgitation.
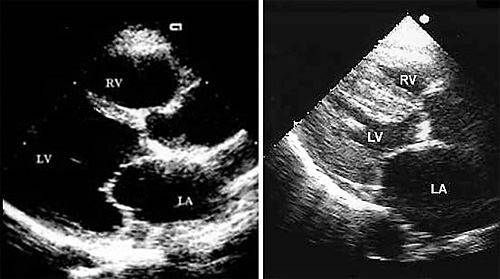
Paradoxical septal motion may also be present. Echocardiography is typically not a key test because windows limit visualizing the right ventricle.
Fatty infiltration of the RV free wall can be visible on cardiac MRI. Fat has increased intensity in T1-weighted images.
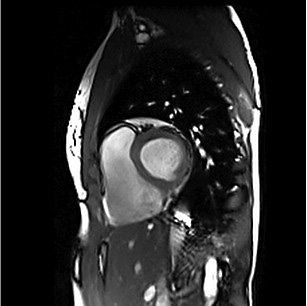
However, it may be difficult to differentiate intramyocardial fat and the epicardial fat that is commonly seen adjacent to the normal heart. Also, the sub-tricuspid region may be difficult to distinguish from the atrioventricular sulcus, which is rich in fat.
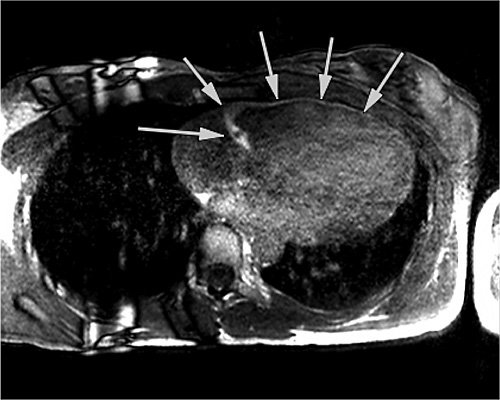
Cardiac MRI can visualize the extreme thinning and akinesis of the RV free wall. However, the normal RV free wall may be about 3 mm thick, making the test less sensitive. Tissue changes are challenging to interpret, but may be a useful adjunct in test interpretation.
Holter monitoring is used to detect ventricular arrhythmias that may be symptomatic or asymptomatic. The number of premature ventricular contractions (PVCs), presence of non-sustained ventricular tachycardia as well as PVC morphology are used to detect and determine the severity of ARVC.
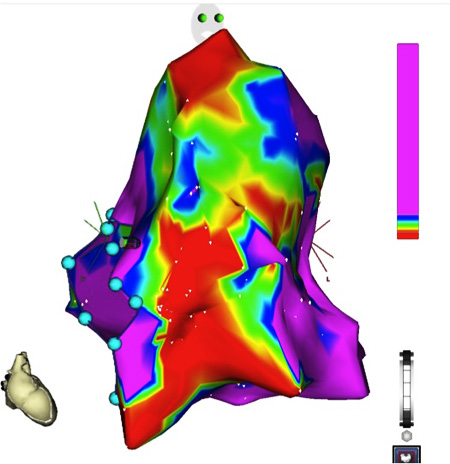
EP testing and voltage mapping are performed to determine if ventricular arrhythmias are inducible with programmed stimulation, occasionally performed in ARVC patients. Voltage mapping looks for areas of low voltage to suggest muscle loss with fat or scar replacement consistent with ARVC, typically in the triangle of dysplasia.
Right ventricular angiography is challenging to interpret. Findings consistent with ARVC are an akinetic or dyskinetic bulging localized to the infundibular, apical, and subtricuspid regions of the RV. The specificity is in the order of 90%; however, the test is observer dependent.
Transvenous biopsy of the right ventricle can be highly specific for ARVC, but it has low sensitivity. False positives include other conditions with fatty infiltration of the ventricle, such as chronic alcohol abuse and Duchenne/Becker muscular dystrophy.
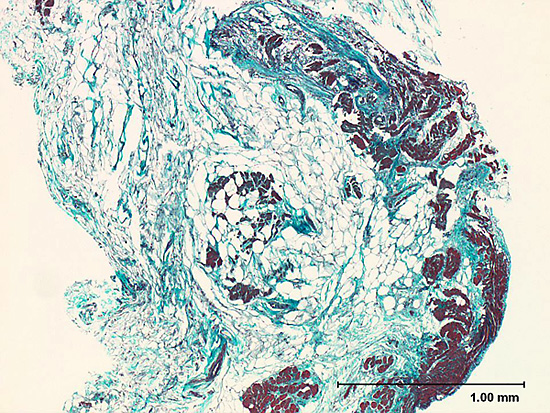
False negatives are common, however, because the disease progresses typically from the epicardium to the endocardium (with the biopsy sample coming from the endocardium), and the segmental nature of the disease. Also, due to the paper-thin right ventricular free wall that is common in this disease process, most biopsy samples are taken from the ventricular septum, which is commonly not involved in the disease process.
A biopsy sample that is consistent with ARVC would have >3% fat, >40% fibrous tissue, and <45% myocytes.