

















Management of ARVC is dependent on the presentation of the patient, test results, risk assessment and patient preference. Exercise has been linked to worsening the severity and progression of disease, so many patients are cautioned against vigorous exercise. If the individual wishes to begin an exercise regimen, an exercise stress test may have added benefit to identify the extent of exercise and heart rate response. Further therapy may include medical management with beta-blockers or antiarrhythmic drugs. ICDs are implanted in high-risk individuals (see below).
Pharmacologic management focuses on arrhythmia suppression. Beta-blockers may play a role in reducing right ventricular stretch, but their benefit is unproven. Antiarrhythmic drug therapy with sotalol or amiodarone is typically considered in patients with established arrhythmias.

While angiotensin converting enzyme inhibitors (ACE Inhibitors) are well known for slowing progression in other cardiomyopathies, they have not been proven to be helpful in ARVC. Individuals with decreased RV ejection fraction with dyskinetic portions of the right ventricle may benefit from long term anticoagulation with warfarin to prevent thrombus formation and subsequent pulmonary embolism.
Catheter ablation may be used to treat intractable ventricular tachycardia. It has a 60-90% success rate.
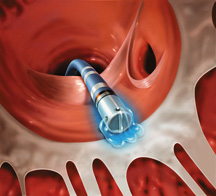
Unfortunately, due to the progressive nature of the disease, recurrence is common (60% recurrence rate), with the creation of new arrhythmogenic foci. Indications for catheter ablation include drug-refractory VT and frequent recurrence of VT after ICD placement, causing frequent discharges of the ICD. Transplantation is rarely performed in ARVC patients
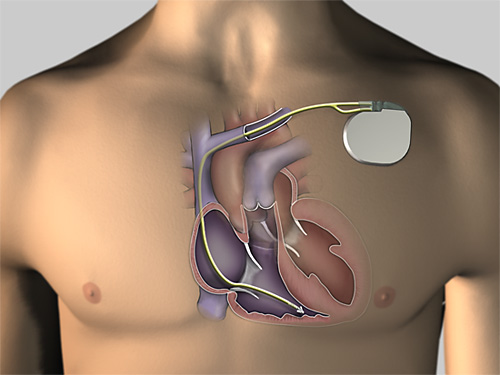
An ICD is the most effective prevention against sudden cardiac death. Due to the risks of surgical implant and implanted system endurance, ICDs are not routinely placed in all individuals with ARVC.
Indications for ICD placement in the setting of ARVC include:
ICDs are often considered in lower risk settings based on individual circumstances. Since ICDs are typically placed via a transvenous approach into the right ventricle, there are complications associated with ICD placement and follow-up. Due to the extreme thinning of the RV free wall, it is possible to perforate the RV during implantation, potentially causing pericardial tamponade. Because of this, every attempt is made at placing the defibrillator lead on the ventricular septum.
After a successful implantation, the progressive nature of the disease may lead to fibro-fatty replacement of the myocardium at the site of lead placement. This may lead to undersensing of the individual's electrical activity (potentially causing inability to sense VT or VF), and inability to pace the ventricle.
Cardiac transplant surgery may be performed in ARVC. It may be indicated if the arrhythmias associated with the disease are uncontrollable or if there is severe bi-ventricular heart failure that is not manageable with pharmacological therapy.
All first degree family members of the affected individual should be screened for ARVC, ideally directed by a health care team with expertise in genetics and cardiology. This is used to establish the pattern of inheritance. Screening should begin during the school-age years unless otherwise indicated. Screening tests include:
The PREPARE study will study 100 patients that carry a gene that can lead to ARVC, but do not have anything more than minor evidence that the condition is present. These patients will not have heart racing on their initial 24-hour monitor. These patients will undergo long term monitoring with an implanted heart monitor that is inserted with a minor surgical procedure, which will detect abnormal heart rhythms that may provide a clue that heart racing from ARVC is present that is not detected with a 24-hour monitor that is performed on an annual basis (St. Jude Confirm implantable loop recorder). These patients will be enrolled in 10 adult and pediatric centers across Canada, and followed for 3 years after their heart monitor is implanted. If heart racing is detected, patients will discuss these results with their doctor to discuss what it means to them. Principal investigator: Dr. Andrew Krahn